Expert consensus on the prevention, assessment, and management of concussion in sport
For over 20 years, a group of global experts on concussion in sport have met every few years to review the research in this field. Based on this evidence, these experts develop recommendations for concussion prevention and the optimization of care for athletes.
The latest International Consensus Statement on Concussion in Sport defines concussion as a “traumatic brain injury caused by a direct blow to the head, neck or body resulting in an impulsive force being transmitted to the brain that occurs in sports and exercise-related activities”
While these recommendations are based on sport-related concussion, many of the same principles apply when assessing and managing any concussion.
Prevention
Recent research has shown that implementing specific policies and procedures that focus on the prevention of concussion reduces the risk of an initial, and recurrent, injury, as well as the potential for persisting symptoms.
the risk of an initial, and recurrent, injury, as well as the potential for persisting symptoms.
Based on this research, the expert panel provided the following recommendations:
- Use mouthguards in child and adolescent ice hockey
- Implement policies that disallow bodychecking in children’s ice hockey and most levels of adolescent ice hockey
- Limit the number and duration of contact practices in American football
- Include neuromuscular training warm ups
- Implement policies that support optimal concussion management strategies (e.g. mandatory removal from play following actual or suspected concussion; clearance from healthcare professional to return-to-play; education of coaches, parents and athletes about concussion signs and symptoms) to reduce recurrent concussion rates
Assessment & Treatment
The diagnosis of a concussion is a clinical judgment, made by a medical professional.
Treatment programs that involved several healthcare professionals seems to be the most effective approach to rehabilitation, and should begin immediately by obtaining a comprehensive history, performing a neurological exam to rule out serious pathology related to traumatic brain injury (TBI) or vascular insufficiency, and screening the cervical spine for signs of trauma.
As a minimum, the health care team involved in the patient’s care should include a family physician and/or sport medicine physician, and a physiotherapist trained in concussion management.
As required, patients may also benefit from a referral to see a psychologist, optometrist or dietician trained in concussion management.
Recommendations
After injury – Initial period (<4 weeks):
- Relative (not strict) rest for 24-48 hours, which includes:
- Limiting physical and cognitive activity
- Limiting screen time
- Start individualized aerobic exercise program 2 days post-concussion. An increase in symptoms is okay if symptoms aren’t reported to be more than 2 points on a 0-10 scale compared to baseline symptoms and they resolve within 1 hour.
- Cervicovestibular rehab with integrated neck and balance interventions should start as soon as 5-10 days after concussion, particularly in patients with headaches, neck pain, dizziness, and balance problems.
After injury – persisting symptoms (>4 weeks):
Collaborative care should be sought and should include exercise rehabilitation, cognitive behaviour therapy, and medication to manage mental health and sleep.
New tools for healthcare professionals that assess concussion
- Concussion Recognition Tool (CRT6) – For use by parents, athletes, coaches. How to use it.
- Sport Concussion Assessment Tool (SCAT 6) – For use by a healthcare professional within 7 days after injury, but best when used within 72 hours. How to use it.
- Child SCAT 6 – More age appropriate for 8-12 year olds. How to use it.
- Sport Concussion Office Assessment Tool (SCOAT6) – 13+ year olds. Comprehensive list of tests, but not a validated tool yet. How to use it.
- Child SCOAT6 – ages 8 to 12. Comprehensive list of tests, but not a validated tool yet. How to use it.

Recovery
To determine how well an athlete is recovering, clinical evaluation and future research should include:
- Patient-reported symptoms at rest, with cognitive activities and following exertion.
- Other outcome measures as related to patient needs such as post traumatic headaches, vestibular ocular reflex, oculomotor function, standing and dynamic balance.
- Measures of return to activity (learning, sport, work).
‘Return to Learn’ and ‘Return to Sport’
Most athletes (93%) fully ‘Return to Learn’ (RTL) (school or work) by 10 days, while unrestricted ‘Return to Sport’ (RTS) may occur within 1 month. These timelines are dependent on how severe symptoms are, pre-existing conditions that may affect recovery (e.g. history of migraines), and postinjury factors (e.g. aggravation of injury, psychological stress).
Research also shows that continuing to play with concussion symptoms and a delay in seeking help from a healthcare professional are associated with longer recovery.
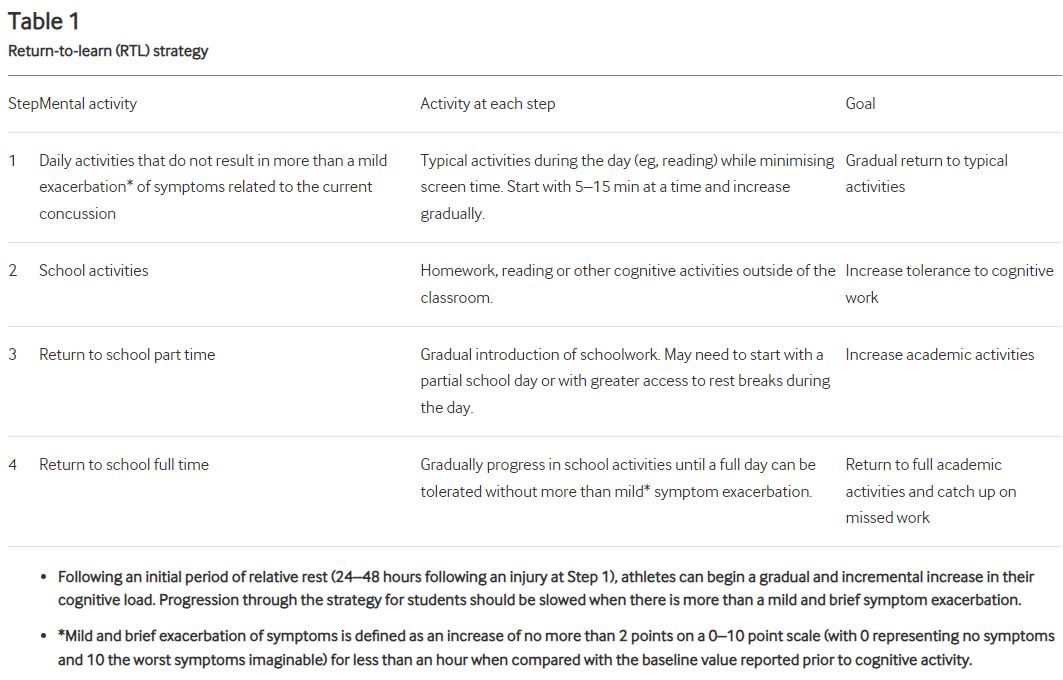
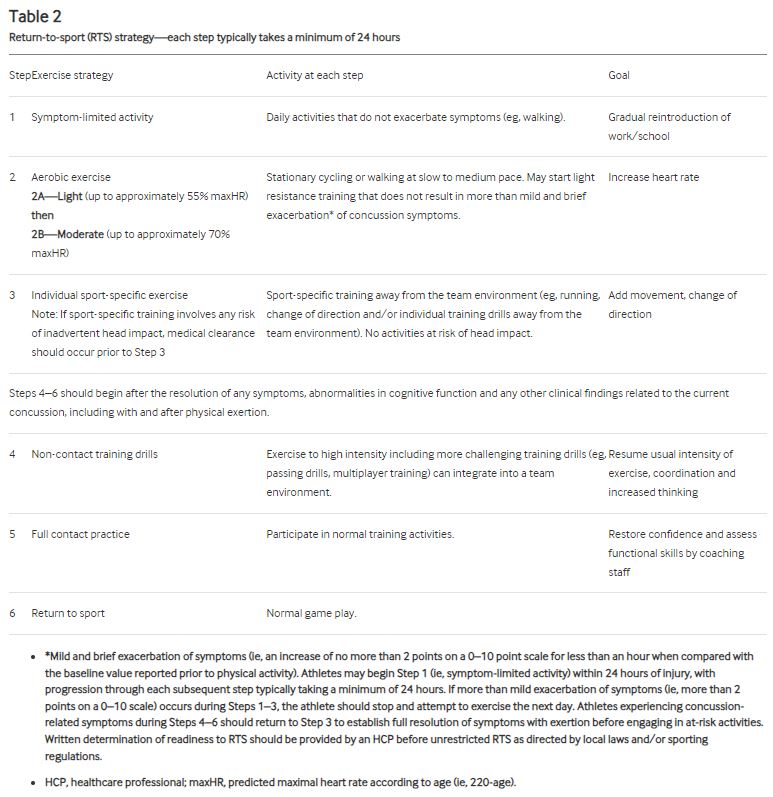
RTL and RTP should follow a graduated step-wise strategy, as described in Tables 1 and 2 below:
In addition to a graduated ‘Return to Learn’, ‘Return to Work’, and/or ‘Return to Play’, patients recovering from concussions seem to benefit the most from specific therapies for the cervical spine, vestibular system, visual system, and cardiovascular system.
Research suggests that focused rehabilitation that begins within the first 7 to 10 days after injury can significantly improve outcomes and decrease long-term symptoms in both children and adults.
Jacob Carter and Ben Lindemulder are physiotherapists at Banff Sport Medicine that are trained in concussion rehabilitation guidelines and techniques.




