Tendon Function and DYSfunction: The Basics
Tendons attach muscles to bones.
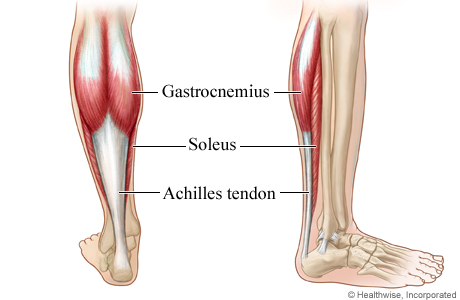
Our two largest calf muscles, the gastrocnemius and soleus are both connected to the heel bone via the Achilles tendon.
They are made of strong fibrous collagen tissue that transmit the force of muscular contraction to a bone in order to create joint motion.
Good quality tendons are like stiff springs. A stiff spring will stretch a little, and then recoil with most of the force that was required to stretch it initially. In our tendons, we call this stretch ‘creep’, and the recoil of the tissue ‘recovery’.
To prevent damage to the tendon, we need to have a certain degree of stiffness, resilience and efficiency.
An example of this would be if I create tension in my calf by hopping on a single leg. The calf muscles transfer this fairly high load to my heel bone via the Achilles tendon. When I do this action repeatedly, a strong tendon can handle the load… whereas a poor-quality tendon may not recover quickly… leading to fatigue of the tissue, and eventually inflammation and micro or macrotearing of the tendon (small tears or a complete rupture).
Areas of tendon pain
This photo illustrates a few of the bursae located around the kneecap (patella). Our body is designed such that any location where there is higher friction between two surfaces, a bursa will typically be present to provide padding and lubrication.
There are three common areas in the tendon where pain can be experienced.
These are in the weakest zones of a tendon where it transitions from tendon to bone, and from muscle to tendon, as well as in the bursa.
Bursa are fluid-filled sacs that protect tendons from the hard surface of bone by acting like a cushion or gliding surface. When there is excessive compression of a tendon on a bursa, the bursa will often become inflamed and irritable. This is more common than you’d expect, and often a diagnosed tendinopathy includes a bursitis.
Common Ways the Tendon Becomes Irritated
Tendons become irritable due to overuse when they are stressed beyond their load tolerance.
Overuse may develop for one of many reasons that include:
1) Excessive volume: Tendons may not be able to adapt to an increased volume of a specific activity (over a period of days/weeks/months)
2) Poor biomechanics: Doing a motion differently than you may have done it previously (over a period of days/weeks/months) may cause irritability, even if the volume hasn’t changed. If you’ve been doing a specific motion with poor biomechanics (i.e. poor form or function) for a while, but then increase the volume, re-read principle #1.
3) Impaired mobility or strength elsewhere: Often, another impairment within close proximity of the tendon may cause you to move poorly, which may ultimately cause you to overuse some parts of your body and under-use others.
4) Excessive stretching: Prolonged and frequent stretching of muscles/tendons may result in excessive creep and poor recovery of the tendon. Subsequent loading of the tendon may then result in increased potential of tendon irritation.
5) Nerve compression: Decreased space at the intervertebral foramen (where the nerves exit your spine), or compression of a nerve by tight muscles may affect the strength of the muscles supplied by that nerve. This may cause poor movement patterns, referred pain, and /or dysfunctional muscle tone that may cause irritation of the tendon.
6) Poor maintenance: Even with reasonable volume and good biomechanics, if you ask your body to perform an activity enough and don’t ensure that the muscles maintain good mobility and tissue quality (e.g. by stretching), the muscles may develop trigger points which in turn will pull on its tendon with increased tension.
7) Other factors: An individual’s risk for developing tendinopathy is also affected by older age, sex, and diseases such as Marfan’s Syndrome, Ehlers–Danlos Syndrome, thyroid disorders, diabetes, rheumatoid arthritis, and having a predisposition to developing kidney stones, gallstones or gout.
Microtearing of the tendon: changes on a cellular level

Yup, this thickened tendon is actually at greater risk of tearing or rupture. It is thicker because of excess inflammation and water, excessive production type 3 collagen fibers and misalignment of the type 3 collagen fibers. Image: www.tonyaanmd.com
Microtearing of tendon fibers occurs with overuse. It results in tendon thickening and can significantly weaken the tendon due to collagen / scar tissue formation.
The result of micro-tearing is a thicker, yet weaker tendon!
The tendon has a greater density of nerve endings which increases the sensitivity to all stimuli including chronic inflammation. Together, these factors create a positive feedback system in which the inflammation irritates the nerve endings, causing increased inflammation… AND the chronic inflammation degrades the quality of the tendon itself. This means that when the tendon is loaded during sports or daily activities, further injury will occur to the tendon, thus creating additional inflammation and pain.
Tendon Take-Homes
Here are a few general principles to keep your tendons happy and healthy:
1) Gradually increase your training volume in anything you do that is physically active.
2) Train regularly, and do not take more than 2 weeks off from strength training, as research has shown that significant decreases in tendon strength can occur.
3) Correct any mobility restrictions, strength impairments, and poor movement patterns that are within your control. Have a good personal trainer, coach, or physiotherapist assess your movement patterns.
4) If you are using your body regularly, use a foam roller regularly (poor man’s massage therapist), and see a body worker (e.g. massage therapist or physiotherapist) for maintenance visits (once a month minimum).
5) Control risk factors that can be changed to avoid developing other health conditions conditions: Eat (mostly) healthy, sleep (mostly) well, and live a happy and stress-reduced life.
When Should I See A Healthcare Provider About My Tendons?
Talk to a healthcare provider straight away if you experience any of the following symptoms:
- Joint or muscle pain that happens suddenly;
- Pain that gets worse;
- An inability to lift or move a part of your body as you usually do.
Without proper treatment and management, and with continued overuse of you tendons, you may develop tendonitis. If you notice ongoing discomfort, see a healthcare provider and learn how to protect your tendons.
This content is based on a previously published article by Jacob Carter Physiotherapy.
Expert Contributor
JACOB CARTER, LEAD



